Inflammation: The Body's 'fire' Burns Threats, But Things Go Wrong When It Smolders
Inflammation: The Body's 'Fire' Burns Threats, But Things Go Wrong When It Smolders
Authored by Flora Zhao via The Epoch Times (emphasis ours),
Many people experience chronic inflammation without even knowing it, Arch G. Mainous III, a professor at the University of Florida (UF) College of Medicine, told The Epoch Times.
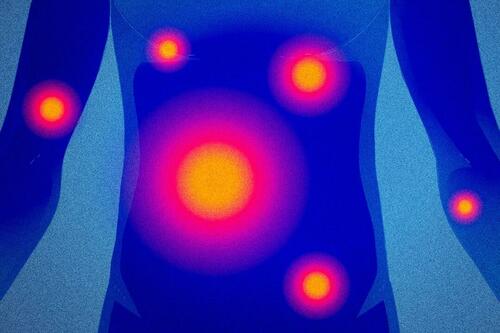
Illustration by The Epoch Times, ShutterstockA large-scale study published in Frontiers in Medicine in 2024 showed that among adults in the United States, almost 35 percent had systemic inflammation. Even among healthy individuals (with no evidence of disease), the proportion was about 15 percent.
Chronic inflammation is linked to a wide range of conditions and often “touches on some big diseases,” Dr. Frank A. Orlando, the medical director of UF Health Family Medicine–Springhill, told The Epoch Times. And its cause lies in what we eat and do every day.
When the Fire Is Allowed to Smolder
“We need inflammation,” Peter Osborne, a clinical nutritionist and chiropractic doctor, told The Epoch Times. The inflammatory response is an essential part of the immune system. When the body is infected or injured, inflammation—often likened to fire—is nature’s way of burning away pathogens and repairing damage. Once the threat is eliminated, inflammation should subside. But if the fire continues to smolder, it can become a chronic issue.
Inflammation that persists for more than three months is chronic inflammation, which triggers heart disease, cancer, diabetes, depression, sarcopenia, autoimmune disease, and neurodegenerative disorders, among others.
Inflammation is the body's immune defense. However, when it persists for more than three months, it becomes a chronic condition. Illustration by The Epoch TimesA review published in Nature Medicine indicated that over 50 percent of deaths can be attributed to inflammation-related diseases.
Chronic inflammation is a significant contributor to many heart diseases. For example, scientists’ understanding of atherosclerosis has evolved from viewing it as a passive accumulation of cholesterol to recognizing it as a condition driven by chronic inflammation. Chronic inflammation triggers biochemical reactions that lead to the formation of atherosclerotic plaques and can cause these plaques to rupture.
A meta-analysis published in The Lancet found that levels of inflammation are linked to increased mortality risk for heart disease, stroke, and several types of cancer. Specifically, every threefold increase in the concentration of C-reactive protein—a standard marker of inflammation—was associated with a 37 percent higher risk of coronary heart disease and a 27 percent higher risk of ischemic stroke.
On the other hand, lower inflammation levels appear to be associated with increased longevity. A study involving hundreds of centenarians in Japan found that inflammation levels were more accurate predictors of longevity than telomere length and better predictors of daily living capabilities and cognitive function in older people than age. The study suggested that “suppression of chronic inflammation could be an essential step towards further improvements in human healthy lifespan.”
Short-Term Solution
Most inflammation can be controlled with medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., ibuprofen, naproxen, and aspirin), steroids, and immunomodulatory drugs. In 2023, the U.S. Food and Drug Administration (FDA) approved colchicine as the first anti-inflammatory drug for heart disease.
But while using anti-inflammatory drugs is common in clinical practice, “there are no guidelines recommending NSAIDs for general use long-term to control chronic inflammation,” said Orlando. He added that even over-the-counter NSAIDs carry risks, such as heart attack, stroke, acute kidney injury, and upper gastrointestinal bleeding, and can interact with other medications.
“We do not want to put people on those [medications] for a long time,” especially when it comes to more potent anti-inflammatory drugs like corticosteroids and colchicine, said Mainous, who is also vice chair for research in the Department of Community Health and Family Medicine at UF.
Osborne, who practices functional nutrition, said that anti-inflammatory drugs can affect gut microbiome health and disrupt the production and absorption of certain nutrients. A deficiency in nutrients responsible for regulating inflammation can, in turn, exacerbate inflammation. For example, NSAIDs may lead to vitamin C deficiency, while corticosteroids can result in vitamin D, calcium, and magnesium deficiencies.
Relying solely on medication won’t lead to resolution, said Osborne.
He highlighted a phenomenon: Developed countries have some of the best health care systems in the world, but when it comes to chronic inflammation, heart disease, diabetes, obesity, autoimmune diseases, and other conditions, “we spend more money trying to treat these diseases, but we fail.”
David Furman, who holds a doctorate in immunology and is the director of the 1000 Immunomes Project at the Stanford University School of Medicine, said that modern lifestyle is a key problem.
While modern technology makes life more convenient and comfortable, this convenience is merely a façade, he said. “We sit for long periods, eat fast food and highly processed foods, and endure high levels of work stress, all of which can trigger and worsen inflammation,” he said.
Unhealthy lifestyles drive chronic inflammation, which leads to a variety of diseases. Illustration by The Epoch TimesDiet Is a Main Driver
“The biggest driver of chronic inflammation is found in our food,” Osborne said.
Food’s role is to nourish the body, providing energy and nutrients to maintain proper function. However, various food additives, such as artificial flavors, colors, emulsifiers, and added sugars, can contribute to chronic inflammation. Studies have demonstrated that common emulsifiers in processed foods, such as carboxymethylcellulose (CMC) and polysorbate 80 (P80), can damage the gut and induce inflammation. Additionally, the high levels of sugar and refined carbohydrates in ultra-processed foods can lead to elevated blood sugar and oxidative stress, triggering inflammation.
A large study published in 2020 found that individuals who followed a pro-inflammatory diet had elevated levels of multiple inflammatory markers and a 38 percent increased risk of heart disease. Another study based on data from the U.S. National Health and Nutrition Examination Survey (NHANES), published in 2022, found that those who consumed a high amount of pro-inflammatory foods had a 41 percent increased risk of cancer mortality.
“You do not eat the food today, and you have a heart attack because of it tomorrow,” said Osborne. The problem is “when you eat poorly day in and day out for decades of your life,” which gradually prevents the body from ceasing inflammation until its defenses break down and disease occurs.
However, Osborne said that doctors in most countries rarely emphasize nutrition. During their eight years of medical education, they receive minimal training in that area. He hopes that diet will become a fundamental component when doctors educate patients on combatting diseases.
Several experts highlighted that avoiding ultra-processed foods is more important than simply consuming foods with potential anti-inflammatory properties. Mainous pointed out that eating a single anti-inflammatory food, such as a specific fruit, may not yield the desired anti-inflammatory effects.
Another important factor contributing to diet-induced inflammation is food allergies.
“There’s an old saying: One man’s food is another man’s poison,” Osborne noted, sharing the story of a patient he helped. The 6-year-old girl, who had an inflammatory disease, was given only six months to live. Fortunately, Osborne discovered that the child was allergic to blueberries, which her mother had been giving her every morning in a blueberry smoothie. Eliminating blueberries from the girl’s diet saved her life.
Gluten and certain substances in soy and milk can also cause inflammation in some individuals, Osborne added. Through modern medical tests and examinations, people can identify their trigger foods and adjust their diets to mitigate and prevent inflammation.
Toxins Inside and Outside Our Homes
Various synthetic ingredients in everyday household items and cosmetics not only directly irritate the skin but can also enter the body, leading to inflammation.
Polyfluoroalkyl substances (PFAS), found in drinking water, cookware, and food packaging, can increase inflammatory responses.
Harmful chemicals also exist in the air we breathe, especially in a bustling metropolis. According to Furman, types of air pollutants such as PM2.5 and PM10 (particle matter with diameters of less than 2.5 micrometers or 10 micrometers, respectively) can cause inflammation in the brain and lungs. Moreover, formaldehyde in new furniture or newly constructed homes can lead to cardiovascular inflammation. Osborne recommends using an air purifier at home as a basic protective measure for people living in areas with poor air quality.
High Body Fat, Low Muscle Mass
A 2021 study found that prolonged sitting raises pro-inflammatory cytokines in older women and lowers anti-inflammatory cytokines in older men. Another study showed that individuals who sit for long periods have elevated levels of various inflammatory biomarkers in their blood.
A sedentary lifestyle leads to more fat accumulation. “Thirty percent of the interleukin-6 in our bloodstream is secreted by fat cells,” said Furman, noting that this substance contributes to inflammation.
Adults who do not exercise also experience a 3 percent to 8 percent reduction in muscle mass every decade. Several experts highlighted and emphasized the anti-inflammatory benefits of exercise and maintaining muscle during interviews.
Greater muscle mass leads to the production of more anti-inflammatory molecules, said Furman.
“You have to think about the muscle as a secretory organ,” he said. Muscles produce and release cytokines and various small proteins into the bloodstream, which systemically reduce inflammation. This secretion is even more pronounced during muscle contractions.
A study conducted in the United Kingdom that tracked over 4,000 adults with an average age of 49 over a 10-year follow-up period found that those who exercised regularly exhibited reduced levels of two inflammatory markers: high-sensitivity C-reactive protein and interleukin-6. Notably, those who engaged in at least 150 minutes of moderate to vigorous exercise per week had the lowest levels of inflammation.
People who exercise regularly have lower levels of two inflammatory markers than people who don't. Illustration by The Epoch TimesMainous recommends aiming for 150 minutes of exercise per week, with the type of exercise tailored to individual health conditions. For young adults, moderate-to-intense exercise can temporarily increase acute inflammatory markers but helps reduce inflammation over the long term. For older adults and those with chronic conditions, it is crucial to avoid overexertion.
A Silent Inflammatory Agent
Experts also highlighted that stress, while intangible and invisible, is a major contributor to chronic inflammation.
One theory behind stress-induced inflammation is that it reduces the sensitivity of immune cells to signals that usually resolve inflammation.
Additionally, “stress causes inflammation by activating the body’s fight-or-flight response, which then triggers the release of what we refer to as pro-inflammatory chemicals and hormones,” Stephen Sideroff, an associate professor in the Department of Psychiatry and Biobehavioral Sciences and the Department of Rheumatology at the University of California–Los Angeles’ School of Medicine, told The Epoch Times.
Sideroff said that the first step in managing stress is to reframe adverse events as positive challenges. He explained that moderate and well-timed stress can be beneficial as it activates the sympathetic nervous system, preparing people to handle threats effectively.
Many people feel powerless against stress, but this mindset contributes to the problem, according to Sideroff. He recommends adopting a growth mindset toward stress: “I have to learn something new if I am going to handle the situation better.” Through this learning process, one can “figure out a better way of dealing with the stressors in one’s life,” he said.
Excessive stress introduces another problem: As we use our energy to manage stress, our metabolism ramps up to produce more energy and directs more blood to the muscles and brain. However, “we all have just a certain amount of personal energy,” Sideroff explained. As a result, the brain reallocates energy from other organs, such as the kidneys, to address immediate needs. This reduces the kidneys’ ability to filter harmful substances from the blood, which can then further trigger inflammation throughout the body. “This is at the heart of one of the ways that stress leads to aging and disease; a lot of the maintenance processes of the body get neglected,” he added.
Letting go of anger and doubt and facing situations with calmness can also reduce inflammation. Sideroff said that these emotions are similar to stress and consume a significant amount of the body’s energy.
“The less we interpret other people’s behavior, the less stress,” Sideroff said. We should be “learning and figuring out all of the ways that we stress ourselves unnecessarily.”
Additionally, it is essential to allow the body’s repair systems more time to heal.
“After a stress is over, we need to give the body the opportunity to recover, to go into the recovery and healing mode,” said Sideroff. One way to achieve this is finding “time in our day where we can say, ‘I am in a zone of safety, or on an island of safety.’” Even just 10 minutes of letting your guard down and relaxing can be beneficial—whether through meditation or relaxation exercises. This activates the parasympathetic nervous system, facilitating the body’s recovery.
A randomized controlled trial showed that even short periods of meditation can improve mental health, decrease pro-inflammatory cytokines, and increase anti-inflammatory cytokines. Experienced meditators exhibited greater resilience and tolerance to stress and stimuli, with lower levels of inflammation in their bodies.
Furman added that the detrimental effects of loneliness should not be underestimated. “People who are socially isolated, lack strong community support, or do not have the care of friends and family experience significantly higher levels of inflammation.”
He said people should choose an anti-inflammatory approach tailored to their individual needs. “It is not a one-size-fits-all,” he added. For instance, someone with a high-stress job—especially if it is their sole source of income—and an unbalanced diet might start by making dietary adjustments and incorporating regular exercise. Additionally, they should focus on strengthening relationships with family and friends to help reduce inflammation.


